In Vitro Fertilization (IVF) is more than just a medical procedure — it is a journey of patience, strength, resilience, and above all, hope. At Tear of Joys, we don’t just celebrate gifts; we honor the emotional stories behind them. And IVF is one of those profound stories where science meets soul and where dreams take the form of tiny heartbeats.
The Emotional Journey of IVF
For couples and individuals facing fertility challenges, the road to parenthood can be filled with silent struggles, unanswered prayers, and emotional hurdles. But IVF offers a glimmer of light through that darkness. It offers the possibility to hold your baby in your arms — a moment worth every injection, every test, every tear, and every sleepless night.
IVF is not just a clinical solution; it is a story of faith. It’s the courage to try again when nature says no. It’s the quiet strength of a woman who undergoes cycles of treatment. It’s the supportive partner standing by her side. It’s the unwavering desire to build a family — no matter how long it takes.
At Tear of Joys, we believe these journeys deserve to be celebrated, honored, and remembered forever.
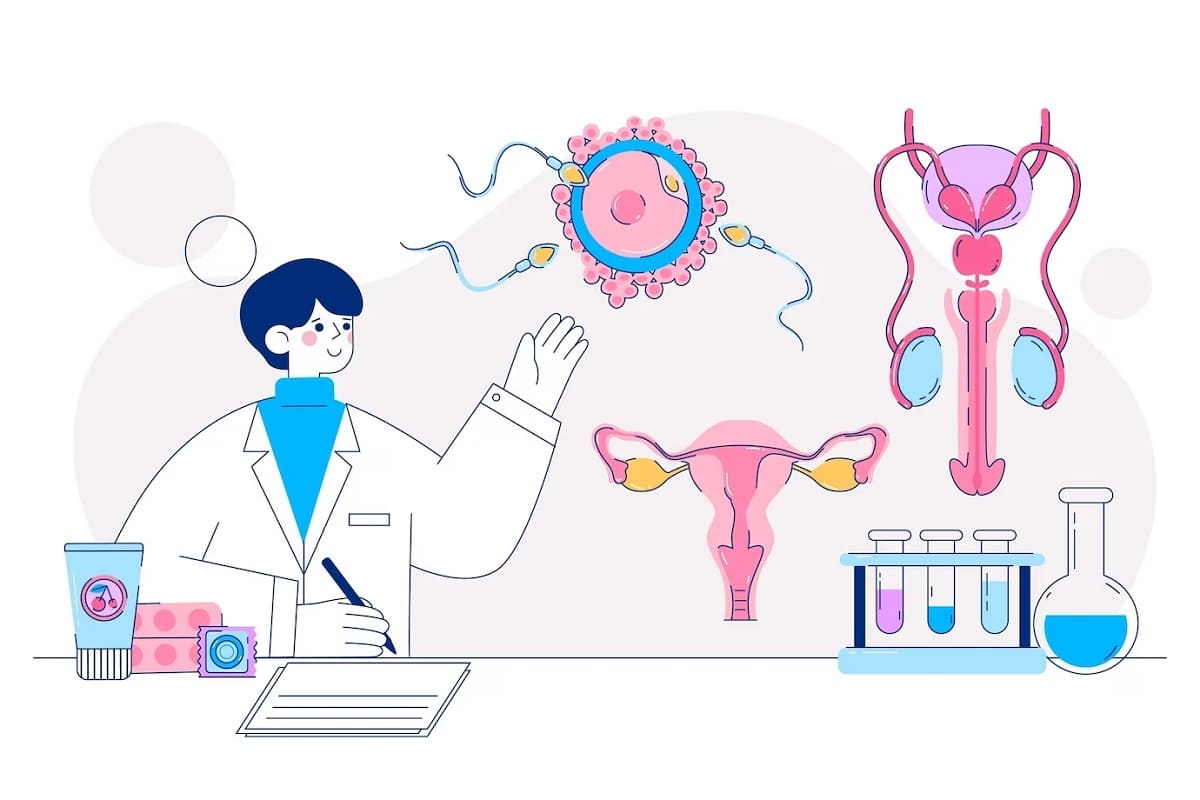
What Is IVF?
In Vitro Fertilization (IVF) is a type of assisted reproductive technology (ART) that involves combining a woman’s eggs and a man’s sperm outside the body in a laboratory. Once fertilization occurs, one or more embryos are transferred into the woman’s uterus, where they may implant and lead to pregnancy.
IVF is often recommended for:
Couples facing infertility
Women with damaged or blocked fallopian tubes
Endometriosis-related fertility challenges
Male infertility issues
Couples with unexplained infertility
Women with PCOS (Polycystic Ovary Syndrome)
Older women seeking pregnancy
LGBTQ+ couples and single parents wishing to conceive
Each IVF cycle is a step forward — filled with hope, uncertainty, and endless prayers.
The Strength Behind the Science
Behind every successful IVF story lies a couple who dared to believe. They’ve endured consultations, hormonal injections, ultrasounds, and the anxious wait for embryo implantation. It’s a journey that tests emotional resilience just as much as physical stamina.
And while science plays a crucial role, it’s the emotional strength of intended parents that truly carries this process. There’s something incredibly beautiful about choosing to fight for your family — against all odds, one embryo at a time.


The Joy of a Positive Test
Ask anyone who has walked the IVF path, and they will tell you: The day you hear your baby’s heartbeat for the first time… is the day your world changes forever.
The joy that floods your heart with that one positive test is unlike anything else. It’s relief. It’s happiness. It’s gratitude. And most importantly — it’s a new beginning.
At Tear of Joys, we have seen so many families express this overwhelming joy through thoughtful gifts — memory boxes to save ultrasound pictures, journals to write down the first heartbeat experience, or personalized baby announcement keepsakes. Because moments like these should never be forgotten.
IVF Is Love in Action
There’s no single definition of family. Some are born easily. Others are built through tremendous perseverance. IVF is a reminder that love creates families, and biology is just a small part of the equation.
The IVF journey teaches us that being a parent isn’t just about giving birth — it’s about believing, caring, sacrificing, and loving with every piece of your being. It’s love in its purest, rawest, and most determined form.
A Gift for Every IVF Story
At Tear of Joys, we’ve created a special collection for IVF warriors and their families. Whether it’s a gift for the soon-to-be parents, a thank-you token for doctors and fertility staff, or a surprise for a partner who stood by every injection and appointment — our curated IVF gifts are designed to reflect the emotion, sacrifice, and triumph behind every IVF journey.
Some meaningful ideas include:
Personalized IVF milestone journals
Engraved ultrasound frame with the baby’s due date
Inspirational quote plaques for fertility warriors
“Worth the Wait” baby announcement boxes
Keepsake boxes for storing IVF memories
Every IVF baby is a miracle. Every couple who makes it through the process is a warrior. Every story deserves to be told.
Let’s Celebrate Your Journey
No matter where you are on your IVF path — beginning, waiting, or finally holding your baby — know that you are seen, loved, and supported. Your strength inspires others. Your journey brings hope. And your story is worthy of being cherished forever.
Let Tear of Joys be a small part of that celebration. Let us help you mark your IVF journey with thoughtful, emotionally rich keepsakes that reflect the miracle you’ve created. Because behind every embryo, every test result, and every tear… is a future filled with laughter, lullabies, and love.

